- CMS has finalized a new episode-based alternative payment model for CABG.
- Selected hospitals in certain geographic regions will be required to report starting in 2026.
- Surgeons and administrators at selected hospitals should begin preparations early.
This month, the Centers for Medicare & Medicaid Services (CMS) finalized a new mandatory episode-based alternative payment arrangement called the Transforming Episode Accountability Model (TEAM).
The TEAM will affect cardiothoracic surgeons who perform coronary artery bypass grafts (MS-DRG 231 to 236) and a limited number of other specialties. Starting in 2026, this approach will be mandatory in 761 hospitals in certain geographic regions. STS provided feedback to CMS, cautioning that if the model is not implemented judiciously, it could change patient care by causing a race-to-the-bottom effect.
Payment
For impacted facilities, the hospital will be responsible for the cost and quality of care for patients who have undergone surgery and the first 30 days after they leave the hospital. During this period, hospitals will continue to submit their usual fee-for-service claims. CMS will evaluate the regular spending on all CABG episodes compared to the target price established beforehand. CMS originally proposed a 3% discount factor for all CABG episodes, but this was reduced to the STS-recommended 1.5% discount factor to prevent a decrease in the quality of care to cut costs.
The target pricing includes the following services:
- Physicians’ services
- Inpatient hospital services
- Outpatient therapy services
- Skilled nursing facilities
- Home health services
- Clinical laboratory services
- Durable medical equipment
- Medications (Part B drugs and biologicals)
- Hospice
Additionally, CMS will measure providers based on two quality metrics:
- All-Cause, Unplanned Hospital-Wide Readmission Measure
- Patient Safety Indicator 90 (PSI 90): Patient Safety and Adverse Events Composite
STS advocates for capturing clinically relevant CABG-specific measures to better capture physician performance. These measures are already being captured in most cardiothoracic surgery departments and would not increase additional administrative burden.
Timeline
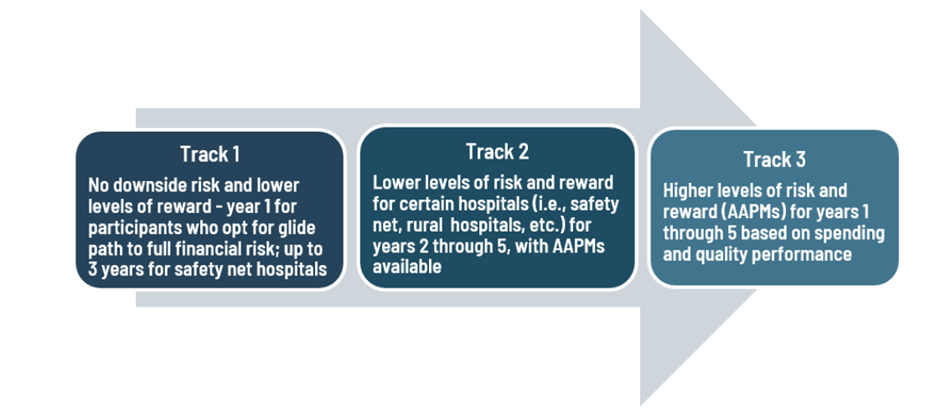
TEAM is a five-year model starting in 2026. Hospitals will assume financial responsibility with three participation tracks:
Preparation for Surgeons and Hospitals
If your hospital is selected for mandatory participation in TEAM, it’s crucial to start preparing now. Carefully review the CMS requirements and discuss them with your hospital administrators and colleagues. Surgeons must stay informed and actively participate in these changes to ensure success under this new model.
STS Action
STS has long expressed our concerns to CMS about requiring physicians to participate in testing unproven payment models. We will continue to advocate for policies that do not inadvertently penalize cardiothoracic surgeons. Many of the details on CMS target pricing have not been released, but STS will provide meaningful feedback to CMS on this topic and share it with membership once it is available. If you have any questions, please contact advocacy@sts.org or refer to these resources:
1 https://www.ebglaw.com/insights/publications/cms-issues-mandatory-team-model-for-acute-care-hospitals-to-improve-episode-based-alternative-payments-and-advance-accountable-care-relationships
