- The Centers for Medicare & Medicaid Services (CMS) has finalized a policy affecting coding and reimbursement for 90-day surgical global periods, effective January 1, 2025.
- Surgeons and staff should familiarize themselves with the details as it may impact reimbursement.
- A 90-day surgical global period is a bundled payment system covering all care related to a surgery, provided by the surgeon or their team, before and after the procedure.
- Modifier -54 is used by the surgeon to indicate they performed only the surgical portion of a procedure, and that care was formally transferred.
The Centers for Medicare & Medicaid Services (CMS) recently finalized a new policy impacting the coding and reimbursements for 90-day surgical global periods. This change may impact reimbursement so surgeons and their staff should learn about the details of this policy going into effect on January 1, 2025.
CMS has had a long, ongoing mission of ensuring that payments to practitioners and the relative values (RVUs) assigned to global surgical packages accurately reflect the resources involved in providing these services. CMS has implemented recommendations and policies to accomplish this, often based on flawed and inaccurate data.
In the latest Medicare Physician Fee Schedule (MPFS CY 2025), CMS has finalized a new policy that requires the use of the Surgical Care Only transfer of care modifier (modifier -54) when billing a 90-day surgical global period for informal transfers of care, in addition to the previous requirement that modifier -54 be used when there is a formal, documented transfer of care. While STS has advised CMS against implementing this policy change because of confusion about the scenarios in which it would apply, CMS finalized it making it necessary for our members to understand it and compliantly code for any 90-day globals.
What are 90-day globals and what is included?
A 90-day surgical global period refers to the bundled payment system used by Medicare and other insurers for certain surgical procedures. The global period is the window of time immediately preceding and following surgery, during which all related care provided by the surgeon or a practitioner from their group is considered part of the surgical fee.
This global fee includes all services related to the procedure provided by the surgeon or a member of their group practice as follows:
- Preoperative Visits: This includes preoperative visits after the decision for surgery is made beginning the day before major (90-day global) or the day of minor (0-, 10-day global) procedures.
- Intraoperative Services: Intraoperative services that are a usual and necessary part of the surgical procedure.
- Complications Management: All additional medical or surgical services treating complications from the surgery (e.g., bleeding, wound infections) that do not require takeback to the operating room or dedicated special procedure room, plus any follow-up visits related to complications from the procedure.
- Routine Postoperative Visits: The usual follow-up visits after surgery to monitor recovery and check for complications. Most cardiothoracic surgery services have daily visits in the hospital, discharge day services and one to two post-discharge office-based E/M visits valued into the 90-day global period.
What is NOT Included: Certain services are excluded from the global period and may be separately billed with appropriate documentation and modifiers if required, including:
- The initial consultation or evaluation to determine the need for surgery for major (90-day global) procedures.
- E/M, critical care, and other services unrelated to the surgical procedure (e.g., management of underlying or co-morbid conditions, unrelated illnesses); diagnostic and radiological procedures.
- If a patient needs a second surgery for postoperative complications that requires a return to the operating room or designated special procedure room, or a procedure clearly unrelated to the original surgery, those services would be separately reimbursed.
- Postoperative care for conditions that arise after the 90-day period ends.
Understanding what is included in the 90-day global period is necessary for proper reimbursement. The 90-day global package is under constant threat from CMS, with CMS believing surgeons are not providing appropriate follow up care to patients. For more information, see CMS's updated Medicare Learning Network booklet on Global Surgery.
What is Modifier -54?
Modifier -54 (Surgical Care Only) is used by the surgeon, appended to the CPT code for the surgical procedure; to indicate they performed only the surgical portion of the procedure and a formal, documented (written) transfer of care was executed. For CY 2025 CMS finalized the requirement that for 90-day global surgical procedures, the use of modifier -54 will also be required in instances when a practitioner only intends to perform the procedure and does not intend to provide or does not anticipate providing the post-operative care, even if no formal transfer of care has been executed.
Modifier -54 should be used for:
- Formal Transfers of Care: If the surgeon and another healthcare provider in another group practice formally agree through written documentation to transfer post-operative care, the primary surgeon should append modifier -54 to the code for the primary procedure (e.g., CABG, lung resection). This indicates that the primary surgeon is not responsible for follow-up care. This policy remains unchanged from past guidance regarding the use of modifier -54.
- Informal Transfers of Care (New!): If the surgeon performing the surgery does not expect to provide follow-up care, modifier -54 should be appended to the primary procedure code (e.g., CABG, lung resection). While STS urged CMS to provide greater clarification regarding what an informal but expected transfer of care was, CMS only clarified that this broadened policy applies to circumstances where “when a practitioner only intends to perform the procedure and does not intend to provide the post-operative care” or “does not anticipate seeing the patient for any follow-up visits.” CMS has not provided guidance on applying modifier -54 if a provider delivers some of the anticipated post-op visits but not all. Without that information, we cannot accurately estimate.
Implications for Surgeons
- Payments Could Be Impacted: Reimbursement to surgeons using modifier -54 will be limited to only the preoperative and surgical portions of the global fee. The provider(s) who deliver post-operative care bill(s) separately for their services. CMS has created a new add-on code HCPCS G0559 for these providers to report with their E/M thereby identifying these visits as post-op.
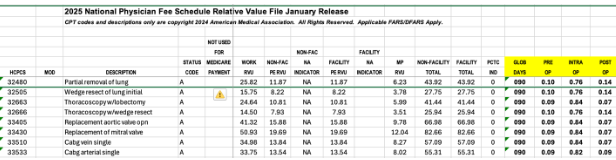
The percentage assigned to the pre-, intra-, and post-operative payment by the procedure can be found in the National Physician Fee Schedule Relative Value File or by using the Medicare Physician Fee Schedule (PFS) Look-Up Tool. The exact reimbursement for providers billing modifier -54 is unclear given that CMS has not clarified when and how to bill modifier -54.
Example:
- Document All Follow Up Care: Include a clear record in the patient’s chart that they have received or are scheduled for all appropriate follow up care within the 90-day global period. This will help avoid any negative impacts of contradictory -55 modifier (Postop management only by a different provider) claims or claims reporting an E/M code with the new post-op visit G-code, G0559 from other providers. Modifier -55 is used as the counterpart to modifier -54; the provider responsible for post-op care who did not perform the surgery would bill this. This will help protect against any potential audits on 90-day globals.
- Use Modifier -54 for all Formal or Informal and Expected Transfers of Care When Billing a 90-day Global Surgery: Surgeons who do not intend to provide post-operative care should coordinate with the provider who will manage the patient’s follow-up visits to the extent possible. This ensures the claims are properly submitted and the post-op services are accurately billed using the appropriate codes and modifiers.
- Exceptions: Modifier -54 typically applies to procedures with 10- or 90-day global periods. While this includes most cardiothoracic surgery procedures, some services such as VADs, ECMO and diagnostic thoracoscopies have XXX or 0-day global periods and as such, the transfer of care modifiers do not apply.
